Medscape Psychiatrist Lifestyle, Happiness & Burnout Report 2023: Contentment Amid Stress
- Deena Terrell, LCSW, BC-TMH
- Mar 1, 2023
- 3 min read
Mary Lyn Koval | February 24, 2023

Psychiatrists are finding that their happiness level and work-life balance are not springing back easily even as COVID-19's effects on the workplace wane. Many doctors are struggling to find the same level of contentment that they enjoyed before the pandemic, to feel like they are healthy people with enough time for their families. Meanwhile, the impact of persistent burnout and depression continues to build among psychiatrists. Frustration, sadness, and anger are widespread. Medscape surveyed more than 9100 physicians across more than 29 specialties. Their responses give insights into how choices surrounding their marriages, family relationships, personal habits, and lifestyles influence their happiness. Psychiatrists also told poignant stories of how burnout and depression affect them, how these challenges can harm personal and patient relationships, and how they are trying to deal with them. (Note: Some totals in this presentation do not equal 100% because of rounding.)

Compare psychiatrists against other specialists in the percentage who said they were either "very happy" or "happy" with their lives away from work before the COVID-19 pandemic hit. At least 3 in 4 physicians in every specialty felt that happy about their personal lives before the pandemic upended American society.

Psychiatrists surveyed by Medscape were as likely as physicians overall (58%) to describe their lives away from the office as "very happy" or "happy." Physicians in every specialty were substantially less happy with their personal lives than they were pre-pandemic.

In last year's Medscape report, 30% of male psychiatrists and 46% of their female counterparts said they felt burned out (either burned out or both burned out and depressed). Burnout consistently afflicts a greater percentage of female physicians overall than male physicians. "Studies have shown a clear link between microaggressions — either race- or gender-based — and an increased risk of workplace distress," says Wendy Dean, MD, co-founder of Fixmoralinjury.org. "Whether it's emotional exhaustion (burnout) from constantly having to defend their authority; being overlooked for leadership opportunities; having different expectations of behavior; being interrupted or talked over in meetings; or as betrayal (moral injury) by an organization failing to uphold stated codes of conduct, women's relative disempowerment to men puts them at higher risk of distress." This year, 36% of physicians overall said they felt burned out, 5% felt depressed, and 18% said both.
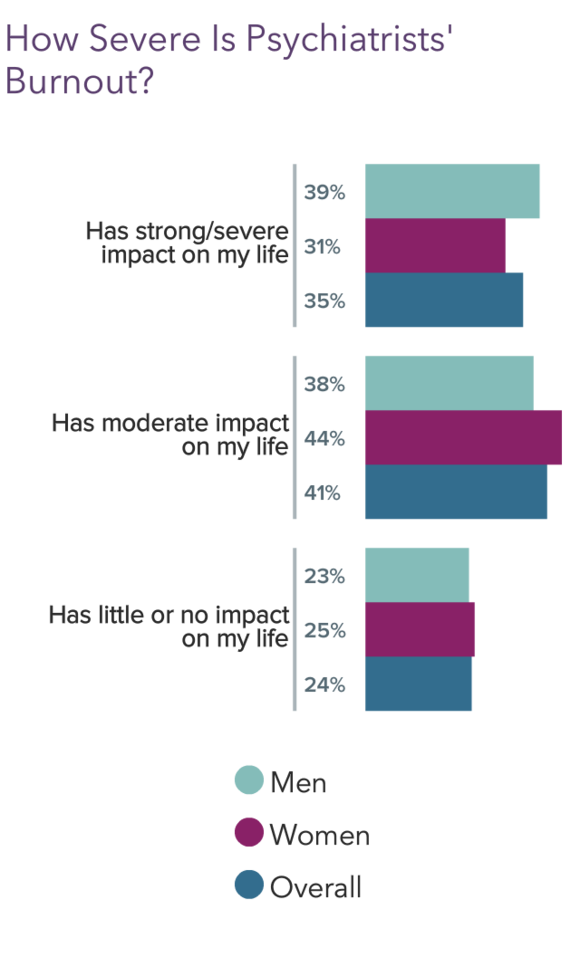
The share of burned-out psychiatrists who cited strong or severe impacts was somewhat smaller than that of physician respondents overall (43%). Meanwhile, 22% of physician respondents in general who said they were burned out reported little or no impact. The largest share of burned-out physicians in general said this year that burnout has a severe impact on their lives. Harvard Business Review noted that there are three types of burnout: (1) Overload, in which you feel forced to work at an unsustainable pace; (2) Underchallenged, where your tasks are boring and monotonous; and (3) Neglect, in which you have no guidance or structure. Overload was mentioned most often by physicians.

In last year's report, the leading factors behind burnout among psychiatrists were (1) bureaucratic tasks, (2) too many hours on the job, (3) lack of peer respect, (4) lack of control or autonomy, and (5) increasing computerization of their practice. EHR documentation continued to frustrate physicians in general. On average, physicians spent 1.84 hours per day beyond work hours completing EHR documentation, according to research published in a JAMA Internal Medicine report. That adds up to 9.2 hours spent each week on work outside of the workday.

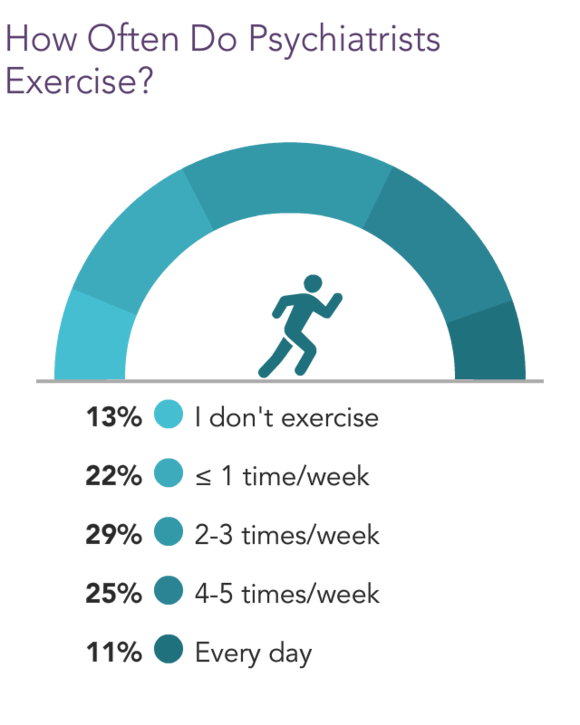
The coping mechanisms most frequently used by doctors overall were (1) exercise, (2) talking with family or friends, (3) getting more sleep, and (4) spending time alone. Physicians overall mostly chose positive coping mechanisms such as exercise and talking with friends, although smaller percentages ate junk food, drank alcohol, or engaged in binge-eating. Some doctors may use a combination of tactics at different times. Other coping tactics mentioned: Read books unrelated to medicine; pray; hunt and fish; take a crafting class; binge on Netflix; play video games; internet shopping and surfing; ride my motorcycle; play with my dog; see a therapist.
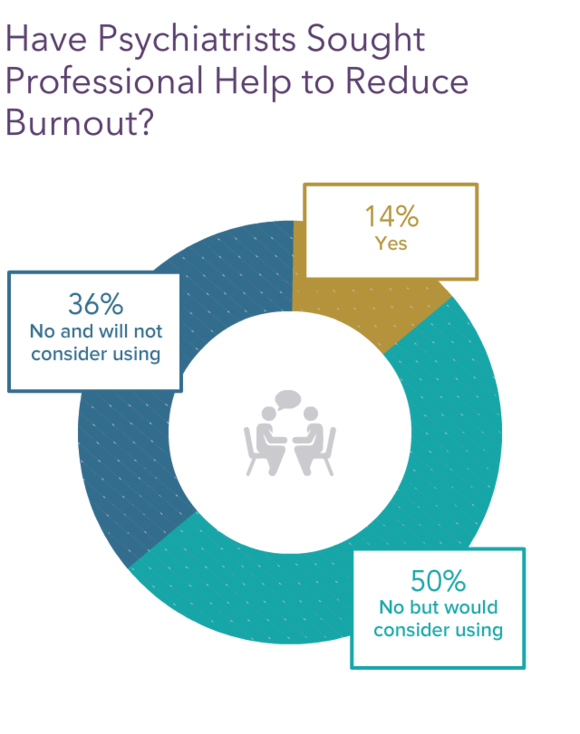
Compare psychiatrists with 13% of all doctors who said they have sought professional help outside of the workplace for burnout. Many physicians commented that they feel that they can deal with it themselves and that professionals have nothing to add.

%201_6_Provider.png)
Comentarios